Dr Kadiyali Srivatsa
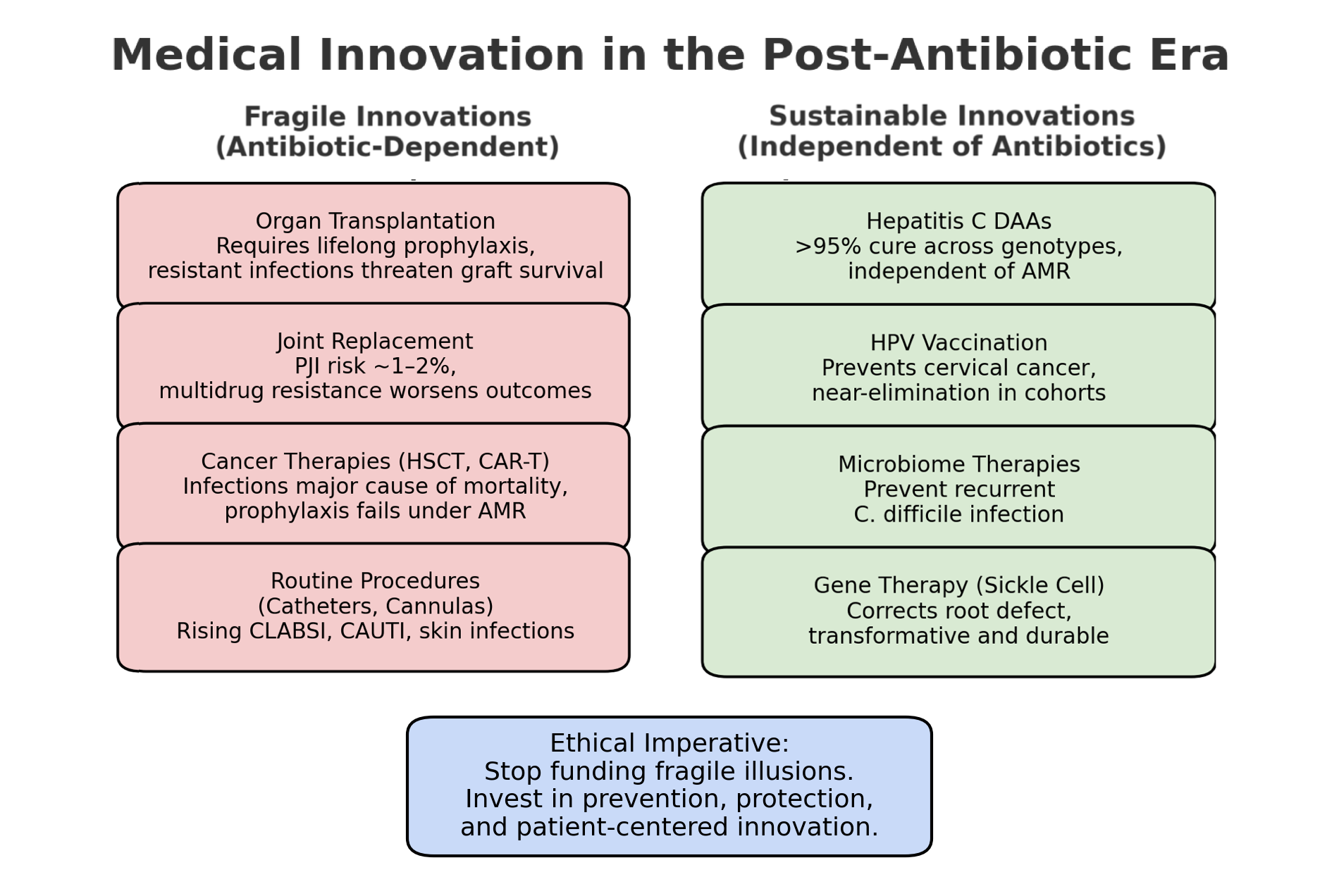
The modern healthcare landscape stands at a critical juncture where the foundations that enabled revolutionary medical advances are increasingly under threat. The user's assertion that many contemporary medical innovations will lose their effectiveness in the post-antibiotic era due to antimicrobial resistance represents a profound challenge that demands careful examination. While antibiotics have indeed been the cornerstone enabling safe invasive procedures, the evidence reveals a complex reality where some innovations have delivered on their promises while others have fallen short, and the emerging antimicrobial resistance crisis threatens to undermine decades of medical progress.
The Historical Foundation: How Antibiotics Enabled Modern Medicine
The relationship between antibiotics and surgical innovation represents one of the most transformative partnerships in medical history. Prior to the antibiotic era, surgical procedures carried enormous risks of infection that often proved fatal. The discovery of penicillin by Alexander Fleming in 1928 and its mass production during World War II marked the beginning of what researchers call the "Golden Age of Antibiotics" from the early 1940s to the mid-1960s[1][2].
The impact was immediate and dramatic. Before antibiotics, surgical site infections (SSIs) were a leading cause of surgical mortality, with infection rates often exceeding 50% for major procedures[3]. The introduction of antibiotic prophylaxis revolutionized surgical practice, enabling complex procedures that were previously considered too dangerous. Cardiac surgery, organ transplantation, joint replacement, and cancer treatments all became viable options once the risk of post-operative infections could be effectively managed[3].
Research demonstrates that approximately 15% of all hospital antibiotics are prescribed for surgical prophylaxis, highlighting the central role these medications play in enabling modern surgical practice[4]. The timing of antibiotic administration has proven critical - giving antibiotics shortly before surgical incision ensures therapeutic levels are present when patients are most vulnerable to bacterial contamination[3].
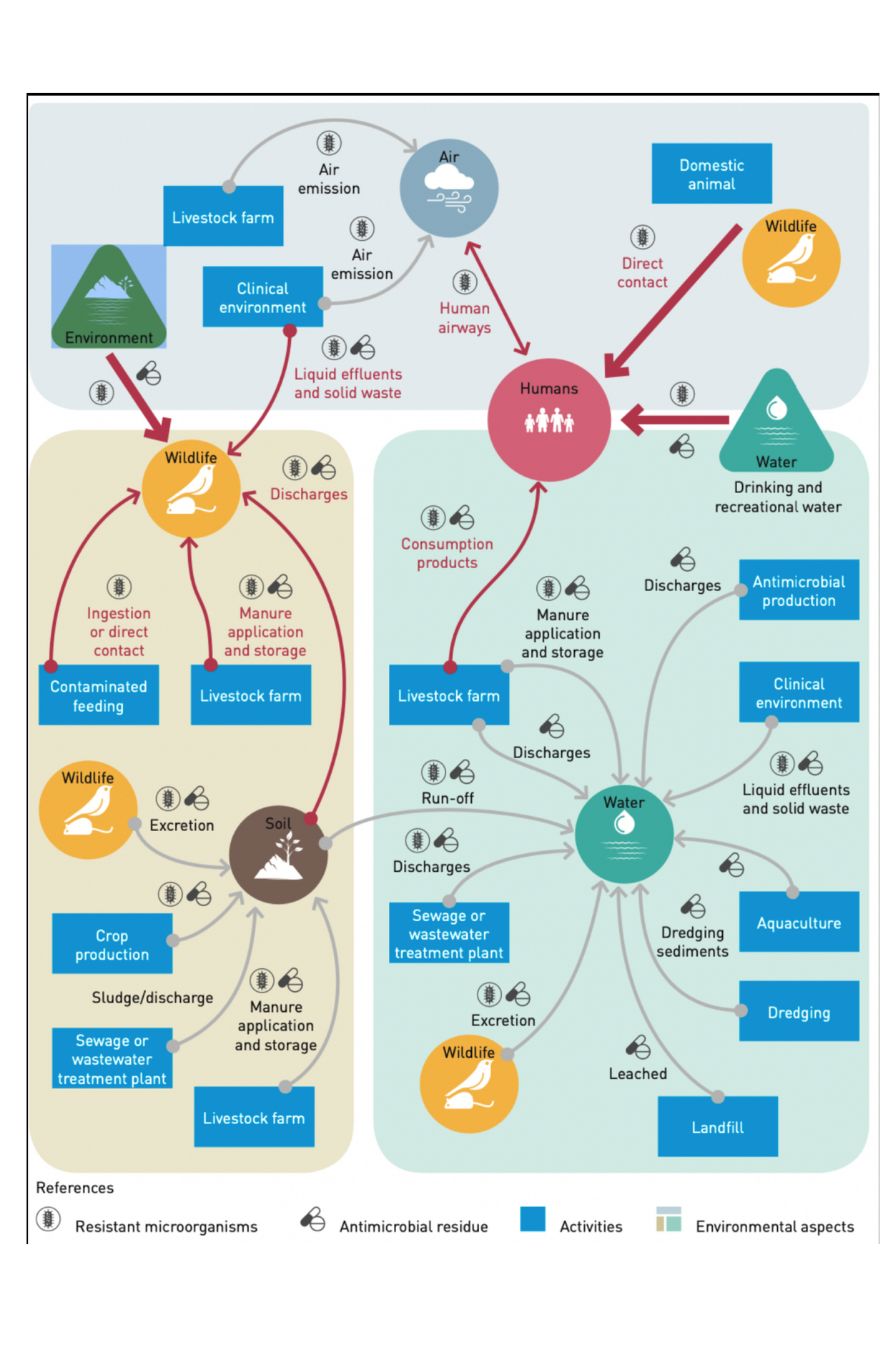
However, this success came with unintended consequences. The widespread use of antibiotics created evolutionary pressure for bacterial resistance, a natural phenomenon that has been accelerated by decades of overuse and misuse[5]. Studies show that 30% to 50% of antibiotic prescriptions are incorrect in terms of indication, choice of agent, or duration[5].

The Current Antimicrobial Resistance Crisis
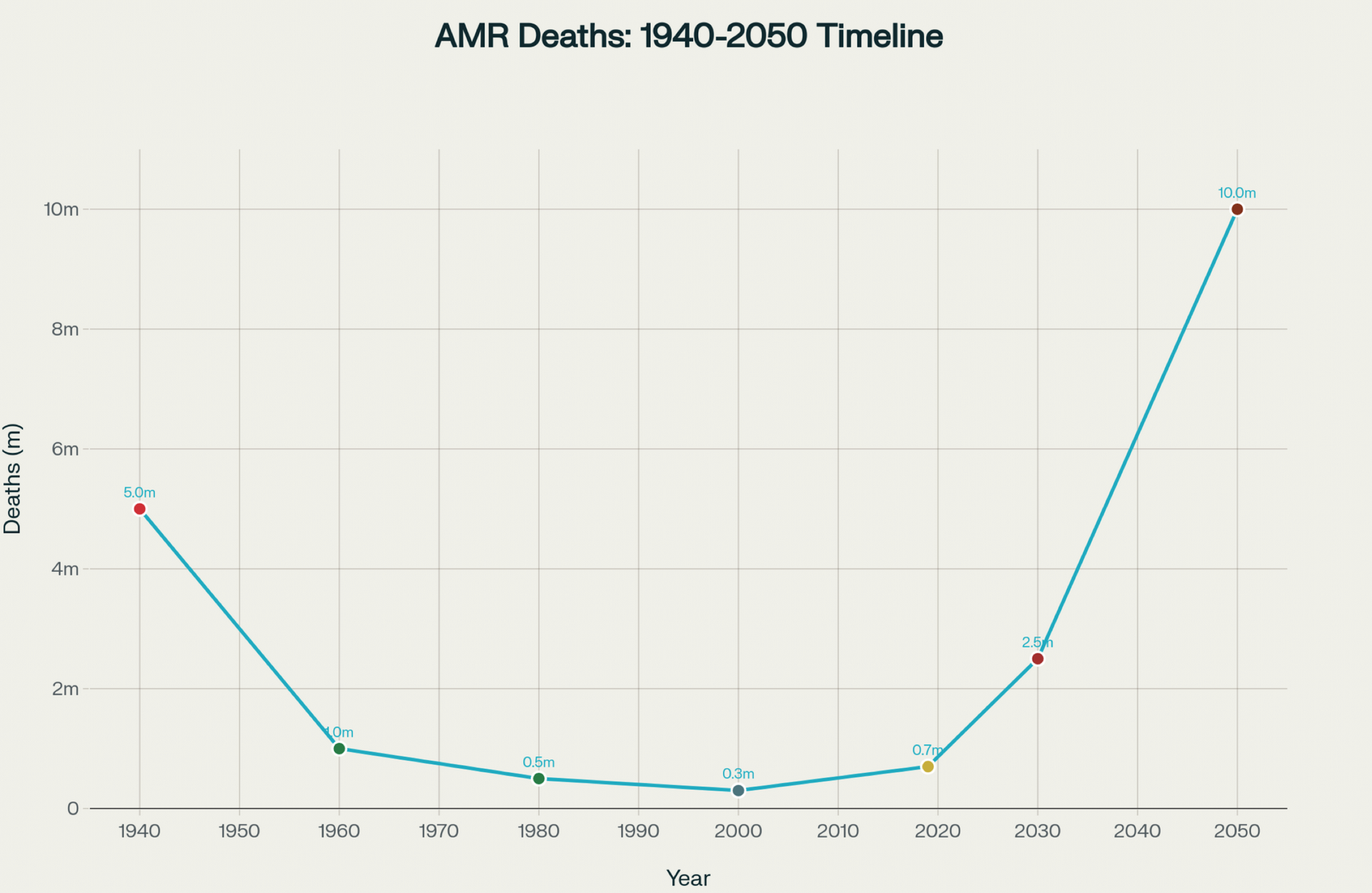
The post-antibiotic era is no longer a distant threat but a present reality. The World Health Organization warns that antimicrobial resistance (AMR) represents one of the top 10 global health threats, with drug-resistant infections currently causing an estimated 700,000 deaths annually[6][7]. Without intervention, this number is projected to reach 10 million deaths by 2050, potentially surpassing cancer as a leading cause of mortality[8][9].
The implications for surgical practice are profound. Research indicates that in some regions, more than half of infections caused by Gram-negative bacteria involve species resistant to carbapenem drugs - the "antibiotics of last resort"[8]. For gastrointestinal surgery specifically, studies show that 21.6% of surgical site infections involve organisms resistant to the prophylactic antibiotics administered, with rates reaching 36% in low-income countries[10].
The economic burden is equally staggering. AMR-related infections increase hospital stays, require more expensive treatments, and result in higher mortality rates. Individual cases of drug-resistant infections can cost healthcare systems between $18,000 to $29,000 more than susceptible infections[11]. The broader economic implications include reduced productivity and increased healthcare costs that threaten the sustainability of modern medical systems[9].
 Evaluating Medical Innovations: Promises Versus Delivered Outcomes
Evaluating Medical Innovations: Promises Versus Delivered Outcomes
Successful Innovations with Proven Value
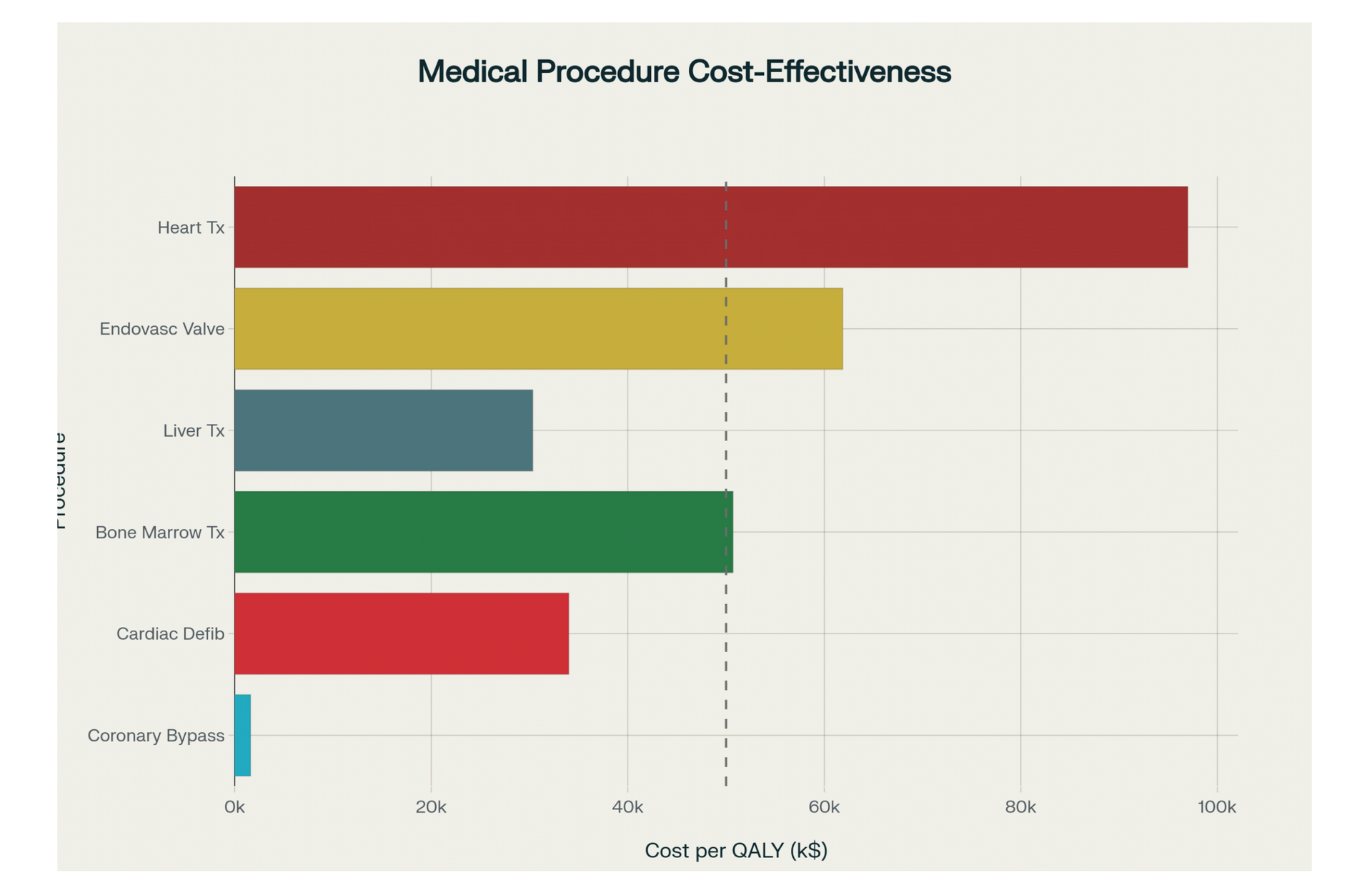
Despite the challenges posed by AMR, many medical innovations have delivered substantial benefits and proven their worth through rigorous cost-effectiveness analysis. Coronary artery bypass surgery exemplifies this success, with studies showing it provides the highest value among costly elective procedures at $1,621 per quality-adjusted life year (QALY) saved[12]. This intervention extends life expectancy by an average of 17.6 years and demonstrates consistent effectiveness across diverse patient populations.
Similarly, targeted cancer treatments like trastuzumab for HER2-positive breast cancer have proven their worth despite initial controversies over cost and access[13]. The drug's clinical effectiveness ultimately justified its widespread adoption, illustrating how evidence-based evaluation can distinguish truly beneficial innovations from marginal ones.
However, the medical literature is replete with examples of innovations that failed to deliver on their promises or caused unintended harm. Research identifies a troubling pattern where unproven innovations often achieve rapid uptake while beneficial interventions remain slow to adopt[14]. Examples include percutaneous bladder neck suspension for stress incontinence, which initially showed promise but demonstrated disappointing long-term outcomes in follow-up studies[14].
The pharmaceutical industry has experienced notable failures, with drugs like Vioxx causing significant harm before being withdrawn from the market[15]. Similarly, advanced medical devices and procedures sometimes show initial promise but fail to demonstrate sustained benefit. Pfizer's inhaled insulin Exubera, despite a decade of development, proved commercially unsuccessful due to its clunky delivery system and potential side effects[15].
The Problem of Unproven and Harmful Innovations
The Challenge of Unnecessary Procedures
Perhaps most concerning is the evidence of systematic performance of unnecessary invasive procedures motivated by financial incentives rather than patient benefit. A comprehensive analysis of 79 cases found that 92.4% of unnecessary procedures were motivated by financial gain, often continuing for five or more years before detection[16]. These procedures not only cause direct harm through physical complications but also erode trust in the medical system and waste precious healthcare resources[16].
Studies using sham-controlled surgical trials reveal that non-specific effects of surgery and invasive procedures are often large, particularly for pain-related conditions where placebo effects can account for 78% of the observed benefit[17]. This research challenges the assumption that invasive interventions are inherently superior to conservative treatments and highlights the need for more rigorous evaluation of surgical procedures.
The Economics of Patient-Centered Versus Doctor-Centered Care
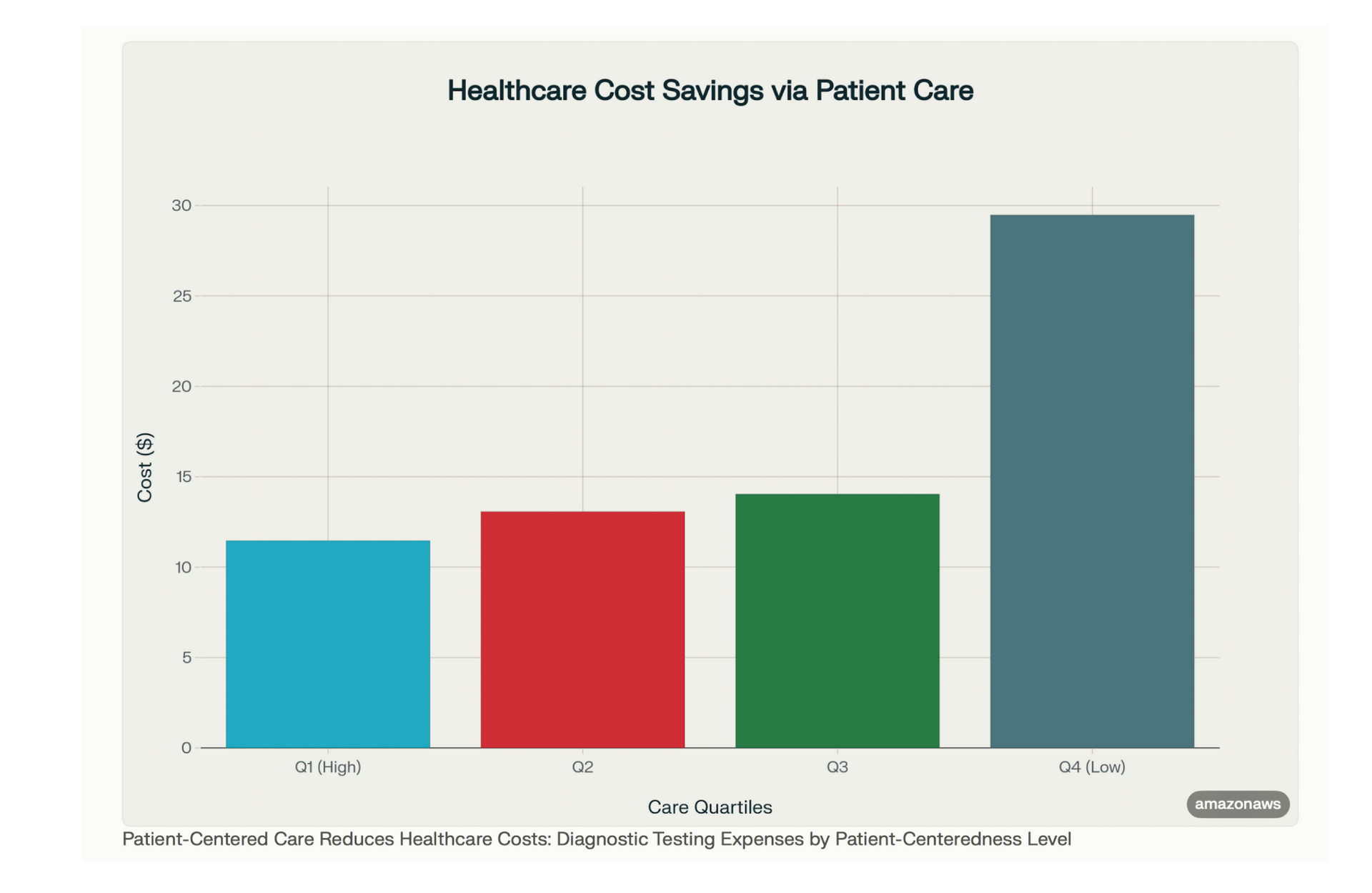
The distinction between patient-centered and doctor-centered care extends beyond philosophical differences to measurable economic impacts. Research consistently demonstrates that patient-centered approaches not only improve health outcomes but also reduce healthcare costs through more judicious use of diagnostic testing and treatments[18][19].
Studies involving 311 family practice patients revealed that higher patient-centered care scores correlated with significantly lower diagnostic testing costs over two months[18]. When projected to national populations, implementing patient-centered care at the highest quartile level could save approximately one-third of diagnostic testing costs[18]. This translates to potential savings of $14 million monthly in Ontario and $38 million in Canada[18].
The mechanism behind these savings relates to reduced information asymmetry between patients and physicians. When doctors engage patients more effectively, explaining treatment options and involving them in decision-making, both parties make more informed choices that reduce unnecessary testing and procedures[19]. This approach also decreases physician-induced demand - situations where doctors order unnecessary tests or procedures based on financial incentives or performance metrics rather than clinical need[19].
Infection Prevention: The Most Cost-Effective Medical Innovation
While many medical innovations struggle to demonstrate clear cost-effectiveness, infection prevention programs consistently show remarkable returns on investment. Hospitals typically achieve 300-500% return on investment from comprehensive infection prevention programs[20]. These programs reduce not only the direct costs of treating infections but also the indirect costs associated with extended hospital stays, additional procedures, and long-term complications.
Healthcare-associated infections add an estimated 7-21 days to hospital stays and can increase treatment costs by $14,300 to $18,500 per patient [21]. In contrast, comprehensive prevention programs including hand hygiene, screening, and isolation measures cost significantly less while preventing multiple infections. For example, a MRSA prevention program costing $167,495 annually generated savings of $851,565 through a 33% reduction in MRSA incidence [21].
The economic case for prevention becomes even more compelling when considering the reduced effectiveness of treatment in the antimicrobial resistance era. Prevention programs that reduce infection rates by 30-70% provide exponentially greater value when treatment options are limited or ineffective [21].
The Sustainability Challenge in Healthcare Innovation
The fundamental challenge facing healthcare innovation is sustainability in an environment of rising costs and limited resources. Healthcare expenditures continue to grow faster than economic growth in most developed countries, with technology being the primary driver[22][23]. While some innovations provide clear value, others contribute to cost escalation without proportional benefits[24].
The fee-for-service payment model incentivizes quantity over quality, leading to overtreatment and inappropriate care[25]. This system rewards procedures and interventions while undervaluing prevention and conservative management. Research suggests that integrated healthcare systems with coordinated care delivery achieve better outcomes at lower costs compared to fragmented systems[25].
Innovation in healthcare must therefore be evaluated not only for clinical effectiveness but also for economic sustainability and societal benefit. The development of expensive treatments that benefit only a small number of wealthy patients while consuming disproportionate resources raises ethical questions about healthcare equity and resource allocation[26][24].
Recommendations for Future Medical Innovation
- Based on this analysis, several key recommendations emerge for ensuring that medical innovation truly serves patient interests rather than commercial ones:
- Enhanced Evaluation Requirements: New medical technologies should undergo more rigorous cost-effectiveness analysis before widespread adoption, similar to the technology assessment programs used in other countries[24]. This includes evaluation of both clinical effectiveness and economic impact across diverse populations.
- Emphasis on Prevention: Given the consistent high returns on investment from prevention programs, healthcare systems should prioritize infection prevention and disease prevention over expensive treatments[20]. This approach becomes even more critical in the antimicrobial resistance era.
- Patient-Centered Redesign: Healthcare delivery should be restructured to emphasize patient-centered care, shared decision-making, and reduced information asymmetry between patients and providers[18][19]. This approach consistently demonstrates both improved outcomes and reduced costs.
- Antimicrobial Stewardship: Comprehensive programs to optimize antibiotic use are essential to preserve the effectiveness of existing antibiotics and support the continued viability of surgical interventions[27][11]. This includes appropriate prophylaxis protocols, rapid diagnostics, and infection control measures.
- Economic Incentive Alignment: Payment systems should be reformed to reward value-based care rather than volume-based care, reducing incentives for unnecessary procedures and promoting cost-effective interventions[25].
Conclusion
The post-antibiotic era presents an existential challenge to modern medicine that validates many of the concerns raised about current medical innovation practices. While antibiotics have indeed been the foundation enabling safe invasive procedures, the rising tide of antimicrobial resistance threatens to undermine decades of medical progress. However, the evidence also shows that not all innovations are equal - some have delivered tremendous value while others have failed to justify their costs or caused more harm than good.
The path forward requires a fundamental shift toward evidence-based, patient-centered approaches that prioritize prevention, cost-effectiveness, and sustainable healthcare delivery. Rather than abandoning medical innovation entirely, healthcare systems must become more selective in adopting new technologies, more rigorous in evaluating their benefits, and more committed to addressing the root causes of antimicrobial resistance through comprehensive stewardship programs.
The choice between continuing on the current trajectory toward ever-more expensive and potentially ineffective treatments, or pivoting toward prevention-focused, patient-centered care, will determine whether medicine can successfully navigate the post-antibiotic era. The evidence strongly suggests that the latter approach offers the best hope for maintaining effective healthcare in an era of increasing antimicrobial resistance and rising healthcare costs.
References:
[1] Antibiotic Prophylaxis in Surgical History - Number Analytics https://www.numberanalytics.com/blog/antibiotic-prophylaxis-surgical-history
[2] What was the Golden Age of Antibiotics, and how can we spark a ... https://ourworldindata.org/golden-age-antibiotics
[3] Antibiotic Prophylaxis in Surgery: Current Insights and Future ... https://pmc.ncbi.nlm.nih.gov/articles/PMC10680052/
[4] Infections in surgery – a key battleground to combat antimicrobial ... http://resistancecontrol.info/2017/infections-in-surgery-a-key-battleground-to-combat-antimicrobial-resistance/
[5] The Antibiotic Resistance Crisis: Part 1: Causes and Threats - PMC https://pmc.ncbi.nlm.nih.gov/articles/PMC4378521/
[6] Welcome to the post-antibiotic era. Will we save ourselves in time? https://med.stanford.edu/news/insights/2019/12/welcome-to-the-post-antibiotic-era-will-we-save-ourselves-in-time.html
[7] Antimicrobial Resistance: A Growing Serious Threat for Global ... https://pmc.ncbi.nlm.nih.gov/articles/PMC10340576/
[8] WHO warns against 'post-antibiotic' era - Nature https://www.nature.com/articles/nature.2014.15135
[9] Antimicrobial Resistance: The risk of undoing modern medicine as ... https://www.genevaassociation.org/publication/health-demography/antimicrobial-resistance-risk-undoing-modern-medicine-we-know-it
[10] The threat of antimicrobial resistance in surgical care https://pmc.ncbi.nlm.nih.gov/articles/PMC10638523/
[11] Antimicrobial Challenge in Acute Care Surgery - PMC https://pmc.ncbi.nlm.nih.gov/articles/PMC9598495/
[12] Value Analysis of the Costliest Elective Lifesaving Procedures at an ... https://journalofscientificinnovationinmedicine.org/articles/10.29024/jsim.2
[13] [PDF] Barriers to innovation in the field of medical devices https://apps.who.int/iris/bitstream/handle/10665/70457/WHO_HSS_EHT_DIM_10.6_eng.pdf
[14] why healthcare needs to rethink its love/hate relationship with the new https://pmc.ncbi.nlm.nih.gov/articles/PMC3066840/
[15] Medical Flops Of The Decade - Forbes https://www.forbes.com/2010/06/17/vioxx-merck-pfizer-healthcare-business-baycol-safety.html
[16] Exploring unnecessary invasive procedures in the United States https://pmc.ncbi.nlm.nih.gov/articles/PMC5735893/
[17] To what extent are surgery and invasive procedures ... - BMJ Open https://bmjopen.bmj.com/content/5/12/e009655
[18] Is Patient-Centred Care Associated with Lower Diagnostic Costs? https://pmc.ncbi.nlm.nih.gov/articles/PMC3107114/
[19] patient-centered care, better healthcare: the association between ... https://pmc.ncbi.nlm.nih.gov/articles/PMC10620693/
[20] Economics Of Infection Control: Costs, Benefits & ROI Explained https://infectionshield.ca/economics-of-infection-control-costs-benefits-roi/
[21] Economic analysis of healthcare-associated infection prevention ... https://pmc.ncbi.nlm.nih.gov/articles/PMC7341040/
[22] Drivers of Health Care Costs: A Physicians Foundation white Paper https://pmc.ncbi.nlm.nih.gov/articles/PMC6179664/
[23] Health Care Costs: More Questions than Answers - NCBI https://www.ncbi.nlm.nih.gov/books/NBK235994/
[24] Medical Innovation: Promises & Pitfalls - Brookings Institution https://www.brookings.edu/articles/medical-innovation-promises-pitfalls/
[25] 9 Reasons for Rising Healthcare Costs - PeopleKeep https://www.peoplekeep.com/blog/nine-reasons-for-rising-health-care-costs
[26] Access to effective but expensive treatments: An analysis of the ... https://pmc.ncbi.nlm.nih.gov/articles/PMC10098599/
[27] Antimicrobial Stewardship in Surgery: A Literature Bibliometric ... https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.847420/full
[28] A brief history of antibiotics and select advances in their synthesis https://www.nature.com/articles/ja201762
[29] Quantifying the primary and secondary effects of antimicrobial ... https://pmc.ncbi.nlm.nih.gov/articles/PMC9413182/
[30] A Brief History of the Antibiotic Era: Lessons Learned and ... https://pmc.ncbi.nlm.nih.gov/articles/PMC3109405/
[31] Origin of Antibiotics and Antibiotic Resistance, and Their Impacts on ... https://pmc.ncbi.nlm.nih.gov/articles/PMC10675245/
[32] Antibiotics: past, present and future - ScienceDirect.com https://www.sciencedirect.com/science/article/pii/S1369527419300190
[33] Why AI Projects Fail in Healthcare — And How to Fix It - Orion Health https://orionhealth.com/us/blog/why-ai-projects-fail-in-healthcare-and-what-to-do-about-it/
[34] The Value of Health in a Cost-Effectiveness Analysis: Theory Versus ... https://pmc.ncbi.nlm.nih.gov/articles/PMC10163089/
[35] Benefits and Harms of Interventions With Surgery Compared to ... https://www.jospt.org/doi/10.2519/jospt.2022.11075
[36] 3 Major Healthcare Innovations That Ultimately Failed ... And Why http://www.verawholehealth.com/blog/major-healthcare-innovations-that-ultimately-failed
[37] How to combat antibiotic resistance in surgery https://infectionsinsurgery.org/how-to-combat-antibiotic-resistance-in-surgery/
[38] Resistance to antibiotics: are we in the post-antibiotic era? - PubMed https://pubmed.ncbi.nlm.nih.gov/16216651/
[39] Antimicrobial resistance - World Health Organization (WHO) https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
[40] What are the Top 3 Drivers of Rising Healthcare Costs? - Jorie AI https://www.jorie.ai/post/what-are-the-top-3-drivers-of-rising-healthcare-costs
[41] The cost-effectiveness of person-centred care provided to patients ... https://www.sciencedirect.com/science/article/pii/S2590229620300034
[42] [PDF] The Costs of Healthcare- Associated Infections https://www.theific.org/wp-content/uploads/2016/04/CostsCh29.pdf
[43] Patient-Centered Care: Definition and Examples - Tulane University https://publichealth.tulane.edu/blog/patient-centered-care/
[44] Why Are Health Expenses Increasing in India? - MrMed https://www.mrmed.in/health-library/health-care/rise-in-health-expenses-india
[45] Medical Costs Are on The Rise - Here's How Health Insurance Helps https://www.nivabupa.com/health-insurance-articles/medical-costs-rise-how-health-insurance-helps.html

