The CDC's Viral Focus Is Blinding Us to What Kills Patients
Why the Real Threat Is Secondary Bacterial Infections—and What We Must Do Now
In 2006, at Medica in Düsseldorf, I displayed a poster at the British Pavilion warning pharmaceutical companies, device manufacturers, and clinicians about a looming threat—not viruses, but secondary bacterial infections. I was met with polite curiosity, but no genuine concern.
The majority of deaths during the influenza pandemic of 1918-1919 were not caused by the influenza virus acting alone, report researchers from the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health. Instead, most victims succumbed to bacterial pneumonia following influenza virus infection. The pneumonia was caused when bacteria that normally inhabit the nose and throat invaded the lungs along a pathway created when the virus destroyed the cells that line the bronchial tubes and lungs.
A future influenza pandemic may unfold in a similar manner, say the NIAID authors, whose paper in the Oct. 1 issue of The Journal of Infectious Diseases is now available online. Therefore, the authors conclude, comprehensive pandemic preparations should include not only efforts to produce new or improved influenza vaccines and antiviral drugs but also provisions to stockpile antibiotics and bacterial vaccines as well.
The work presents complementary lines of evidence from the fields of pathology and history of medicine to support this conclusion. "The weight of evidence we examined from both historical and modern analyses of the 1918 influenza pandemic favors a scenario in which viral damage followed by bacterial pneumonia led to the vast majority of deaths," says co-author NIAID Director Anthony S. Fauci, M.D. "In essence, the virus landed the first blow while bacteria delivered the knockout punch."
This has been going on, and on when pandemics occured, and we were lucky because the antibiotics helped us cure the infections, but now antibiotic resistant bacterias are hard to kill, so be prepared for a pandamic that can kill one in 3 people similar to what happenedbefore.
In 2006, at Medica in Düsseldorf, this poster was displayed, warning about Pandemics, and mentioned it will be "Mystery Illness" caused by SARS. Yes my intuition told me, and it was COVID-19, or also known as SARS-2. Now I am saying the next pandamic will be vius follow by a bacteria and fungus that will spread

Nearly two decades later, our children face a deadlier future, not because of wars or climate disasters, but because of evolved, antibiotic-resistant organisms that have adapted faster than we can respond. Once a common bacterium, Staphylococcus aureus has become a global arms dealer, sharing plasmids with bacteria, fungi, and parasites. What was once curable is now lethal.
As a doctor with over forty years of experience on the frontlines—especially in intensive care—I have watched how these infections spread, how systems cover up failures, and how leaders ignore the obvious signs of collapse, despite my tireless work to raise awareness, including publishing books, research articles, podcasts, and videos, the medical community continues to procrastinate, trapped in the illusion that a vaccine or miracle antibiotic will be discovered using AI technology, and we will be free from disease.
As doctors, we make diagnostic and management errors and try to justify or rectify them. In the past couple of decades, this has escalated to a catastrophic proportion, making "Medical Errors" the third most common cause of death.
"Unethical Medical Practice" triggered me to challenge my profession.
The CDC and global health agencies continue to channel enormous funds into virus-centric solutions—developing vaccines, antivirals, and detection tools. However, during COVID-19, most patients didn't die from the virus. They died with it—killed by secondary bacterial infections, leading to multi-organ failure and sepsis. This is well documented, and for years, we have always prescribed antibiotics to patients diagnosed with a viral infection, hoping the antibiotics would prevent secondary bacterial infections.
One overlooked gateway for these deadly infections is something doctors do thousands of times a day: IV cannulation. It's seen as routine and low-risk, and so it is ignored. Both solutions are designed for real-world use, not academic applause. These are tools for prevention, not just treatment.
The Real Emergency
What killed patients during the pandemic wasn't just COVID—it was sepsis, systemic inflammation, and antimicrobial resistance (AMR). And unless we shift the narrative and funding priorities, millions more will die unnecessarily in the next global health crisis. I cringe when people tell me stories about how my healthy childhood friends died in the hospital, why, because I know the death was preventable.
In my article "Superbug Pandemic and How to Prevent Them," published in American Interest in 2017, I said that only a few non-medical professionals know that antibiotics are the foundation of nearly all modern medicine. Cancer therapy, organ transplants, surgeries, minor and significant, and even childbirth rely on antibiotics to prevent infections. Now that the majority of common infections are untreatable, the advances in modern medicine we have made over the past fifty years will come to an abrupt halt.
"Not Music to Your Ears"
If you are a parent investing all your money in the hope that your son or daughter will grow up and have a better life than you, please think again. Severe sepsis after sustaining cuts, bruises, and even a thorn prick can develop Antimicrobial resistance in bacterial wound, skin, soft tissue and surgical site infections.
Pharmaceutical companies have not invested or developed any treatment that can cure any disease, including antibiotics, since the 1970s, because the ROI on investment is zero. Yes, bacteria develop immunity faster than we can discover or produce antibiotics, this is a war that we cannot win, but be “Smart” you can prevent getting infected.
Women were said to have better immunity and so were protected from infections in the past, but now ARM and even viruses have developed an affinity towards women. E. coli, a sexually transmitted disease that cannot be cured, will soon confine women at home, and also stop procreation.
Warned leaders, the CDC, the WHO, the NHS and the Royal Colleges about the Threat to humanity in 2016
We need to:
- Stop treating secondary infections as an afterthought.
- Identify an area where infections are spreading and stay away.
- Invest in point-of-care diagnostics, safe cannulation devices, and AI triage systems.
- Build infrastructure that prevents, not just reacts to, health emergencies.
Empower people to make informed decisions - "Learn, Prevent and Protect Humanity"
"I urge the CDC, WHO, and global leaders to look beyond the virus. The real threat is already inside our hospitals—and spreading, and doctors are not sharing information"
Sexually Transmitted Infections, UTI, and Common Infections are Untreatable!!!
Let's stop pretending we don't see it.
We estimated all-age and age-specific deaths and disability-adjusted life-years (DALYs) attributable to and associated with bacterial AMR for 22 pathogens, 84 pathogen–drug combinations, and 11 infectious syndromes in 204 countries and territories from 1990 to 2021. In 2021, we estimated 4·71 million (95% UI 4·23–5·19) deaths were associated with bacterial AMR, including 1·14 million (1·00–1·28) deaths attributable to bacterial AMR. Trends in AMR mortality over the past 31 years varied substantially by age and location. These bacteria infect more healthy adults and children, and people have been made to beleive they infect vulnerable adults and senior citizens, which is not true.
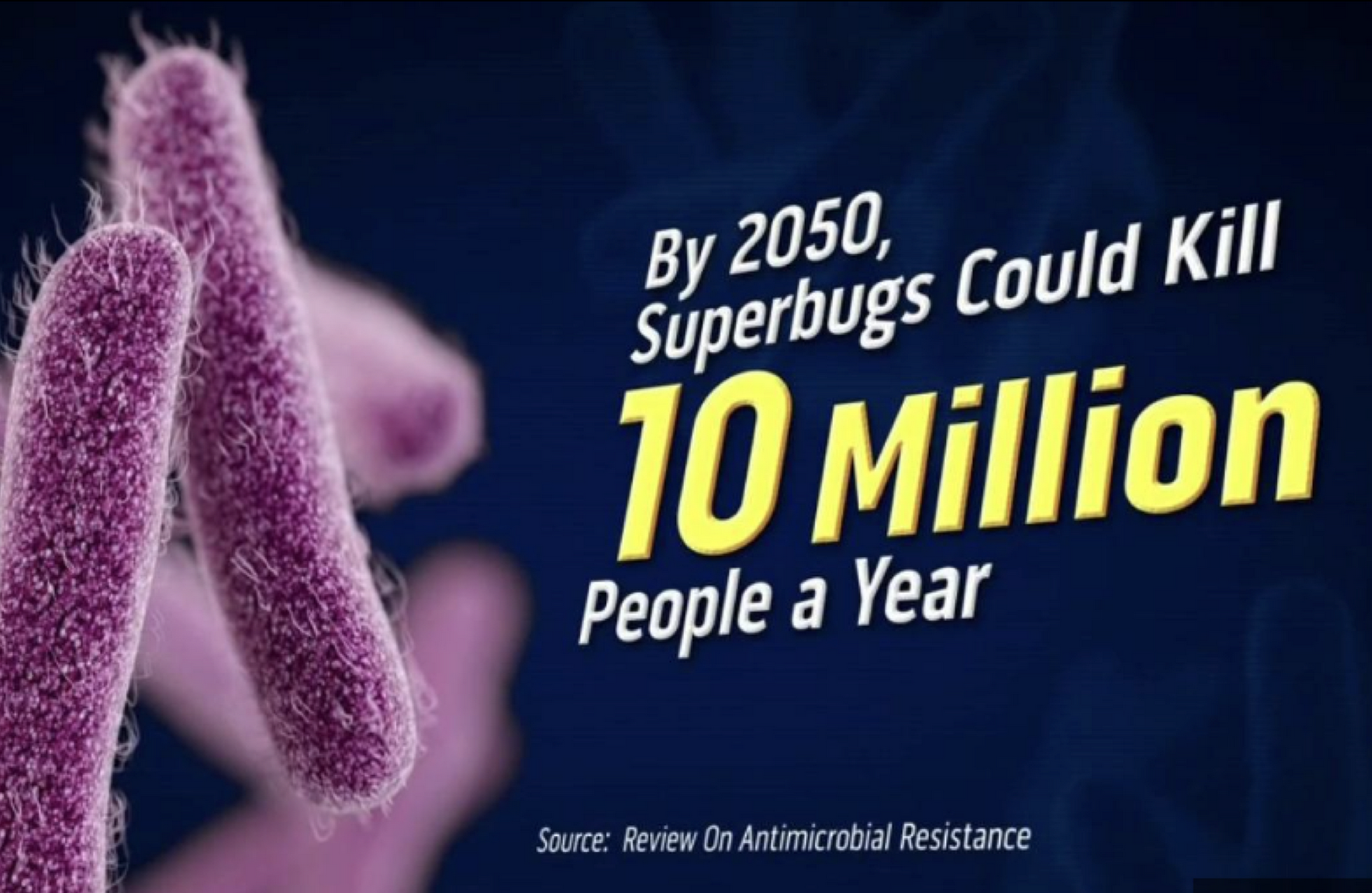
Antimicrobial resistance (AMR) is a significant global health threat and a major health crisis. Due to emerging infectious diseases, the number of people affected is anticipated to increase to 10 million by 2050. Patients with antimicrobial-resistant (AMR) bacterial infections may experience higher morbidity and mortality than do patients with antimicrobial-susceptible bacterial infections, resulting in increased risk of severe, extended illness or death.
AMR makes infections more challenging to treat and makes other medical procedures and treatments significantly riskier. It makes certain bacterial infections difficult or impossible to treat. Treating resistant organisms often requires less readily available, more expensive, and more toxic drugs. In some cases, strains have become resistant to all available antimicrobial agents.
Common and deadly antibiotic-resistant bacteria include Escherichia coli, Staphylococcus aureus, C. diff, Drug-resistant gonorrhea, Methicillin-resistant Staphylococcus aureus (MRSA), multidrug-resistant Mycobacterium tuberculosis (MDR-TB), and Vancomycin-resistant Enterococci.
MRSA kills more Americans each year than HIV/AIDS, Parkinson's disease, emphysema, and homicide combined. In the U.S., 11,285 deaths per year have been attributed to MRSA alone.
Drug-resistant M. tuberculosis infections are difficult to treat. Pseudomonas, CRE bacteria, and Candida auris (fungus) have spread worldwide in India and China. They colonised medical equipment like stethoscopes, percussion hammers, aura scope, tuning forks, syringes, gloves, gowns, furniture, bed linen, X-Ray equipment, scanners, laparoscopes and even hospital walls. It is impossible to sterilise the area because antiseptics and chemicals can only kill sensitive bacteria, not antimicrobial-resistant bacteria, and fungi. Over-enthusiastic sterilisation using strong chemicals helps fungus spread faster, infecting adults and children in hospitals.
I feel sad when leaders like Mr Modi encourage entrepreneurs and medical device manufacturers to invest in and develop medical devices when doctors like me are trying to reduce the equipment and devices used in health. 2. IV Cannulation as a Route for Infection and Sepsis:
Intravenous (IV) cannulas (or peripheral venous catheters, PVCs) are the most widely used invasive medical devices in hospitals, and up to 90% of hospitalised patients require them. Intravascular devices have significant potential for producing iatrogenic diseases resulting in catheter-related bacteraemia or candidemia. Catheter-related bloodstream infection (CRBSI) is a significant clinical problem. It is a type of nosocomial infection that can result in local or systemic infections.
Microorganisms can gain access to the bloodstream via IV devices. The injection ports of peripheral IV cannulas have the potential for microbial contamination. One study found microbial growth on 5.61% of injection port samples from peripheral IV cannulas. Staphylococcus aureus was the predominant organism, accounting for 64% of the microbial growth.
CRBSI can lead to prolonged hospital stay, morbidity, and mortality. Each new episode of CRBSI increases the risk of septicaemia by 4–14% and death by 12–25%. PVC-related bloodstream infections (BSIs) are rarer than other complications like phlebitis or extravasation, but their consequences are potentially severe. The occurrence of PVC-related BSIs has been associated with increased duration of hospital stay, mortality, and costs.
In a study of PVC-related BSI, major complications were noted in 9 out of 25 patients, including severe sepsis requiring ICU admission, mitral valve endocarditis, and a deep pre-sacral abscess. Staphylococcus aureus was the microorganism responsible in all these cases. Six cases (24%) out of 25 in the study died during their hospital stay. While BSI accountability for mortality is difficult, in at least one patient, death was directly attributable to the catheter-related bloodstream infection complications.
Hospitals are settings where infections and superbugs can easily spread among many patients. Healthcare-associated infections (HAIs), many caused by antibiotic-resistant pathogens, result in a large number of deaths annually in the U.S., with sepsis and pneumonia alone responsible for significant fatalities and costs.
WHO Predict 10 million death every year by 2050
3. Challenges of IV Access in Epidemics/Pandemics and Link to Delays and Death:
Why and How Major Device Manufacturers Stifle Innovations to Protect ROI
Please click here to listen to the podcast that will help you learn more.
During the Ebola crisis and again in COVID-19, healthcare workers struggled to find veins for IV access, especially in challenging patients like those who were dehydrated or critically ill with collapsed veins. The inability to insert an IV cannula on the first attempt during the Ebola epidemic led to prolonged patient contact and exposure to contagious fluids. Healthcare workers were disproportionately affected by the Ebola outbreaks, and a significant portion of them died. In the 2014-2016 West African Ebola outbreak, a considerable number of healthcare workers were infected and died.
Many patients died during the Ebola epidemic because IV access could not be secured in time to administer life-saving rehydration fluids and medications. Failed cannulation attempts cause trauma, delays, and increase the risk of infection, which can result in death.
4. IV Access as a "Gateway" and the Need for Innovation in the Context of AMR:
IV cannulation is a "gateway to life-saving care", including fluids, antibiotics, anesthetics, nutrition, and blood. Failing here means "failing at the first step of treatment".
In a world where antimicrobial resistance (AMR) is rising and pandemics are inevitable, "every puncture matter[s]". The severity of complications from PVC-related BSI warrants preventive measures. Investing in prevention, including improved training and high-quality materials/technologies, would be a better use of resources than treating complications.
Innovative cannulation technology is needed to minimize trauma, delays, and infection risk. Organizations like the CDC and WHO warn of future pandemics potentially compounded by AMR, making safe, rapid, and minimally invasive IV access essential. The sources advocating for new technology urge manufacturers, hospitals, and regulators to support innovation, prioritising insertion success and infection prevention. While the sources do not explicitly state that secondary bacterial infections are the primary cause of death during epidemics and pandemics overall, they provide strong evidence that:
AMR bacterial infections are deadly and contribute significantly to global mortality. Infections acquired in healthcare settings (HAIs), including sepsis and pneumonia, are significant causes of death.
IV cannulation is a known route for bacteria to enter the bloodstream, leading to BSIs and CRBSIs, which are associated with severe complications, sepsis, increased morbidity, and significant mortality. Difficulties with IV access during epidemics can lead to delays in administering critical treatments, including fluids and medications (which would encompass antibiotics for bacterial co-infections or secondary infections), contributing to death.
Future pandemics are expected to occur in a context of rising AMR, making the treatment of secondary bacterial infections increasingly challenging and potentially impossible. Therefore, while the sources confirm that preparing for primary viral threats in pandemics is a focus, they also robustly support the notion that secondary bacterial infections, particularly resistant ones exacerbated by healthcare factors like IV access complications, represent a severe threat that contributes significantly to mortality and warrants urgent attention and innovation, especially in contexts like epidemics and pandemics.
Based on the sources provided, here is the information relevant to your query about secondary bacterial infections as a major cause of death during epidemics and pandemics due to IV cannulation leading to sepsis:
Antimicrobial resistance (AMR) is a significant global health threat, contributing to increased morbidity and mortality from infections that are difficult or impossible to treat. Patients with antimicrobial-resistant bacterial infections may experience higher morbidity and mortality compared to those with susceptible infections. AMR is anticipated to increase in the coming years, and AMR bacteria were directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths. Hospital-acquired infections (HAIs), many caused by antibiotic-resistant pathogens, result in a large number of deaths annually in the U.S.. Sepsis and pneumonia, common HAIs, were responsible for a significant number of deaths and costs in 2006. Sepsis is a severe bloodstream infection when bacteria spread to your blood.
Intravenous (IV) cannulas are an integral part of patient care and are a potential route for microorganisms to enter the bloodstream, leading to local or systemic infections. Microorganisms causing vascular catheter-related sepsis can access the bloodstream through the skin at the catheter insertion site or through the catheter hub. The injection ports of peripheral IV cannulas have the potential for microbial contamination. Studies have shown microbial growth on peripheral IV injection ports, with Staphylococcus aureus being a predominant organism.
Catheter-related bloodstream infection (CRBSI), a type of nosocomial infection, is a significant clinical problem that can prolong hospital stay, morbidity, and mortality. While the incidence of local or bloodstream infections associated with peripheral IV cannulas is generally lower than with central venous catheters, their increased frequency of usage means they can considerably prolong hospital stay, morbidity, and mortality. Despite a relatively low incidence of PVC-related BSIs (around 0.2% reported in one study and consistent with others), the total number of PVCs used worldwide suggests the total number of PVC-related BSIs is significant, possibly close to or greater than CVC-related BSIs.
In a study on PVC-related BSI, major complications occurred in nine patients, including severe sepsis, mitral valve endocarditis, and a deep pre-sacral abscess. Staphylococcus aureus was the microorganism responsible for these severe complications. Six out of 25 cases (24%) in this study died during their hospital stay, with one death directly attributed to the catheter-related bloodstream infection. The study notes that the' high incidence and severity of these secondary complications warrant preventive measures.
Factors contributing to microbial transfer and infection via IV cannulation include poor training in aseptic techniques, inconsistent application of skin antisepsis, and disregard for manufacturer-recommended drying times for antiseptics. Combining insufficient drying time with failed cannulation attempts can lead to microorganisms transferring into the bloodstream, causing sepsis. Hospitals are settings where infections and superbugs can easily spread among many patients.
During the Ebola crisis and again in COVID-19, healthcare workers struggled to find veins for IV access, especially in challenging patients like those who were dehydrated or critically ill with collapsed veins. Difficult IV access during the Ebola epidemic meant IV access could not be secured in time to administer life-saving rehydration fluids and medications (which can include antibiotics), contributing to patient deaths. The trauma caused by failed attempts is considered dangerous.
In a world where AMR is rising and pandemics are inevitable, the sources emphasise that "every matter" as cannulation is the gateway to life-saving care, including fluids, antibiotics, anaesthetics, nutrition, and blood; failing here means failing at the first step of treatment.
While the sources strongly indicate that IV-related infections are severe, they contribute to mortality in general hospital settings (including from sepsis). The difficult IV access during epidemics/pandemics can lead to fatal delays in administering necessary treatments (which would consist of antibiotics for secondary bacterial infections); however, they do not provide direct evidence to prove that secondary bacterial infections, introduced explicitly via IV cannulation, are the primary cause of death during epidemics and pandemics.
The sources we reviewed, focusing on potential future pandemics, identify respiratory viruses as the primary threats. However, the material underscores that IV access is critical for treating infections (including bacterial ones) during these crises, and complications with IV access or IV-related infections represent significant risks in such scenarios.